Falls in the Nursing Home
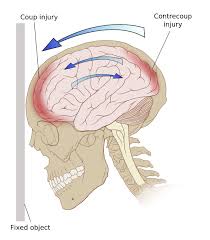
Coup contrecoup
Leslie was performing her 6 AM med pass in the nursing home where she worked when a C.N.A. came to her, breathless, announcing that Mr. Logan tried to get out of bed again, alone, and was on the floor. As they hurried down the hall together, the aide further stated that she had been next door, and heard a thud. She was able to rush right in. He had landed on his buttocks, with his arms and legs spread out.
To Leslie’s question regarding what had happened, he stated, “I needed to use the bathroom and forgot to call for help, I’m sorry—I feel OK, though I landed on this mat and nothing hurts, except my pride.” Leslie performed a head to toe assessment and found no physical injuries. She assisted the C.N.A in getting Mr. Logan up off the floor, onto his feet, and into the bathroom. Mr. Logan avoided a catastrophic head injury.
Falls in the nursing home happen all too frequently. Unfortunately, not all of them end as uneventfully as the scene described above.
Research statistics show that one in three nursing home residents fall annually.
As a gerontological nurse, when I hear that one of my residents fell, my first thought is hoping for no injury or, at least, only bruising. My next thought: “Were all his fall precautions in place?”
As a legal nurse consultant, what items would be at the top of your list to investigate? Consider:
- was there any intervention that should have been ordered but not present?
- has there been a pattern to Mr. Logan’s falls related to time, shift, place, activity, caregiver?
- anything else?
Why do older adults have falls in the nursing home?
There may be subtle changes in adults’ organ systems as well as the presence of medical diseases of an acute or chronic nature that contribute to falls in the nursing home. Experts agree that it is the comorbidity of aging related to changes and not age per se that increases the risk of falls. Here are some of the visual and neuromuscular changes experienced by older adults.
- Visual changes in the older adult include presbyopia – a reduction in accommodation. The effects of presbyopia are most obvious when descending the steps. Because of this condition, older adults may miss the last step (an important reason why the hand-rail must end on the landing surface).
- Changes in the diameter of the pupil, a condition called “senile miosis”, results in smaller pupils. Dimly lit rooms and hallways or surface edges that do not have bold contrasting colors can lead to trips and falls.
- The presence of a cataract, more prevalent in older age groups and with certain conditions, obstructs central vision and can contribute to falls when steps or obstacles are not visualized.
- Some older adults do not lift their feet high. If a reduced steppage height is evident, stumbles, trips and falls can occur when ascending steps or while walking on uneven surface. Also, transitioning from a flat floor surface to a thicker carpeted surface can produce similar falls. Neuromuscular changes include impaired ability to react to sudden loss of balance (from a push or trip) or impaired ability to maintain upright stance.

These steps are dangerous because the railing does not include the last step

Sarah Jean
Fisher
Portions of this blog post came from The Falls Handbook, a guide written to help LNCs analyzes falls cases.
